The Shape of Global Health
Finance & Development, December 2014, Vol. 51, No. 4
![]() WHO on silent killers
WHO on silent killers
![]() Black dog of depression
Black dog of depression
The world has come a long way, but still has a long way to go

THE Ebola outbreak has dominated global health news for much of the second half of 2014. This is understandable given the gruesome nature of Ebola virus disease and its lethality, the current absence of a vaccine or cure, and the prospects for Ebola’s rapid and widespread transmission in the presence of weak and slow-to-react local, national, and global health systems—magnified by the prospect of human error.
Ebola also has the potential to impose a heavy economic burden on affected countries and to cause panic and promote political and social instability in already fragile settings. Ebola conjures up comparisons with other killer infectious diseases—like bubonic plague, smallpox, polio, influenza, and HIV.
But notwithstanding past major assaults on, and contemporary threats to, public health, it is important to remember that humanity has made huge achievements in the prevention and management of infectious disease. These advances have been due in large measure to increased access to clean water and sanitation, the development and widespread use of safe and effective vaccines, revolutions in medical diagnosis and treatment, and improvements in nutrition, education, and income. Health systems—the combination of people, formal rules and institutions, informal practices, and other resources that serve the health needs of a population—have also made significant contributions. Especially effective are systems that emphasize disease prevention, aim for universal coverage, and capably conduct surveillance to detect actual and potential threats to public health—promoting better health behaviors and higher health standards and training, retaining, motivating, and enabling health workers.
Health is indisputably a fundamental aspect of well-being, and there are myriad pathways through which its protection and promotion improve human welfare, both for individuals and for societies. Future perils notwithstanding, technological and institutional innovations hold much promise for making the world healthier, wealthier, and more equitable and secure. Health spending is more than a burdensome consumption expenditure, it is an investment in productivity, income growth, and poverty reduction.
Adding years
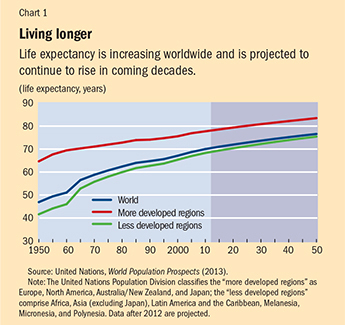
One of the clearest indications of advances in health is the sharp improvement in how long people live. Over the past six decades, global life expectancy has increased more than 23 years and is projected by the United Nations Population Division to increase almost another 7 years by 2050 (see Chart 1). The chart estimates how long children born in a specified year would be expected to live if they were subject to that year’s age-specific mortality rates for their whole life. The steady increase in life expectancy between 1950 and 2010 reflects a sharp drop in infant and child mortality (the infant mortality rate declined globally from 135 per 1,000 live births in 1950 to 37 in 2010) and longer life spans of adults. Life expectancy hovered around 25 to 30 years throughout most of human history, so recent and projected gains rank among humankind’s greatest achievements.
Nevertheless, the economic and fiscal implications of the improvements in life expectancy, and the meaning of longer lives for human welfare, are unsettled. Researchers present a mixed picture of whether postponing death also postpones the age at which people’s minds and bodies begin to break down and they lose their functional independence.
Although living longer may not always mean living better, life expectancy gains are a hopeful indicator of what is possible in the face of both long-standing and new health threats. These threats include infectious diseases like Ebola, malaria, tuberculosis, HIV, hepatitis, diarrhea, and dengue (including drug-resistant forms of these and other pathogens), as well as chronic infirmities such as cardiovascular disease, cancer, respiratory disease, diabetes, neuro-psychiatric conditions, sense organ disorders, and musculoskeletal disorders.
In 2013, 6.3 million children died before reaching their fifth birthday. That represents a decline from 90 child deaths per thousand live births in 1990 to 46 in 2013. Although this is a major improvement, even this lower level of early childhood deaths highlights a major failing of health systems. Most early childhood deaths can be prevented based on existing knowledge and relatively inexpensive interventions such as vaccination, oral rehydration, improved nutrition, access to contraception, use of insecticide-treated bed nets, improved prenatal care, and reliance on skilled birth attendants. Unintended pregnancies are also an important factor contributing to infant and maternal mortality. Unplanned pregnancies were estimated to account for 40 percent of the 213 million pregnancies that occurred globally in 2012. Thirty-eight percent of these unplanned pregnancies resulted in births, which accounted for a disproportionate share of the roughly 300,000 estimated maternal deaths caused by complications in pregnancy and childbirth.
Noncommunicable diseases
The campaigns that led to the eradication of smallpox and the near-eradication of polio are generally regarded as the most successful public health interventions ever. But the lessons these eradication efforts offer for battling noncommunicable diseases, which account for almost two-thirds of the world’s estimated 53 to 56 million deaths a year, are not altogether clear.
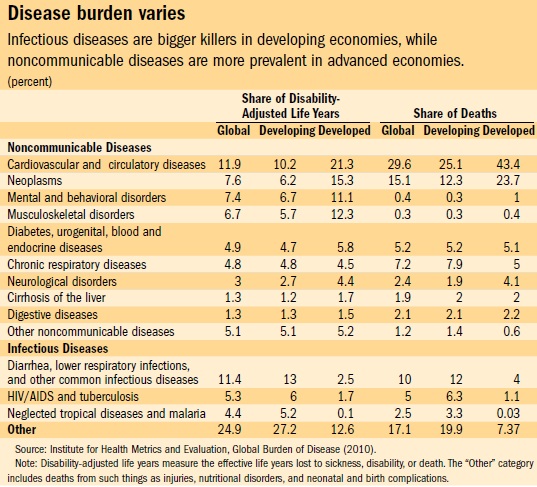
That is because death, or its prevention, is not the only issue in dealing with noncommunicable diseases. A healthful lifestyle is also important. The disability-adjusted life year (DALY) measures the effective years lost to disability and premature death. The table depicts the distribution of deaths and DALYs by cause—globally, and broken down by developed and developing countries. Infectious diseases account for disproportionately more deaths in developing countries, while noncommunicable diseases are relatively more prominent in developed countries. This contrast reflects a phenomenon known as the epidemiological transition. While the transition is a sign of progress, because infectious diseases tend to strike early in life, the fact remains that many deaths from noncommunicable diseases are premature in the sense that they occur before age 70. Some developing countries, such as Bangladesh and Ghana, are only midway through their epidemiological transition and face a heavy dual burden of infectious and noncommunicable disease. Among noncommunicable diseases, cardiovascular and circulatory diseases are the dominant cause of death, followed by cancer. DALY measures indicate that mental illness is also a notable contributor to the global burden of disease—with corresponding adverse implications for labor productivity and quality of life.
Noncommunicable diseases are expected to account for a growing share of the overall disease burden—both from aging populations and from the bad effects of tobacco use, physical inactivity, poor diet, and harmful alcohol use.
There are 967 million adult smokers in the world (18 percent of the adult population), with nearly 6 million tobacco-related deaths each year. Rates of tobacco use are highest in eastern Europe and east and southeast Asia. Tobacco is also consumed in smokeless form, mainly in south and southeast Asia. Although the global rate of smoking (and also the number of cigarettes consumed per smoker) has decreased by about 10 percentage points since 1980, the number of smokers has increased because of population growth. The leading cause of illness and mortality associated with tobacco use is chronic obstructive pulmonary disease, which is responsible annually for an estimated 3 million deaths and 77 million DALYs. Lung cancer is responsible for 1.5 million deaths and 32 million DALYs. Generally, women have much lower rates of smoking than men, although the gender gap has narrowed in recent decades.
Sedentary behavior
The growth of service sector employment, at the expense of agriculture and industry, has been marked and widespread in recent decades and has been accompanied by a rise in sedentary behavior. The shift is magnified by the increase in the proportion of the world population living in urban areas, where there are often fewer opportunities for physical activity. In 1950, 30 percent of the world lived in urban areas; today 54 percent do (see “Moving on Up,” in this issue of F&D). The World Health Organization estimated that in 2008, 31 percent of adults worldwide were insufficiently physically active.
As people eat fewer fruits and vegetables and more refined starch, sugar, salt, and unhealthful fats, there has been a rise in the number of overweight or obese adults (from 29 percent of the global population in 1980 to 38 percent in 2013) and children (from about 10 to 14 percent in the same period). Weight issues contribute to high blood pressure, high blood sugar, and high cholesterol, as well as increases in cardiovascular disease, diabetes, and certain cancers.
Alcohol consumption is growing globally, especially in China and India. Many populations exhibit high rates of heavy episodic drinking that contribute to cirrhosis of the liver, heart disease, cancer, and injury. Binge drinking rates are quite high in Ukraine and Russia and tend to rise with per capita income across countries. Roughly 6 percent of global deaths are attributable to alcohol (7.6 percent among men and 4 percent among women).
Unsettling disparities
In many respects, the most jarring features of the global health scene are the massive disparities between our achievements and failings. For example,
• There is a 38-year gap between the country with the longest life expectancy, Japan at 83 years, and that with the lowest, Sierra Leone at 45.
• Fourteen countries have a life expectancy at birth of less than 55 years, while 25 have a life expectancy greater than 80 years.
• Life expectancy has increased in every wealthy industrialized country over the past two decades, but has declined in five African countries: Botswana, Lesotho, South Africa, Swaziland, and Zimbabwe—mainly because of HIV-related deaths.
• Nineteen countries have an infant mortality rate greater than 60 per 1,000 live births, while in 32 countries fewer than 4 infants die out of each 1,000 live births.
• Ninety-nine percent of child deaths occur in low- and middle-income countries.
• The rate of child mortality in low-income countries is 12 times higher than in high-income countries.
• Globally, women can expect to live over four years longer than men. But that difference is less than two years in 24 countries, presumably a reflection of a preference for sons that manifests itself in mistreatment of female children, gender-based violence, and gender inequities, such as restrictions on women’s access to adequate nutrition and health care.
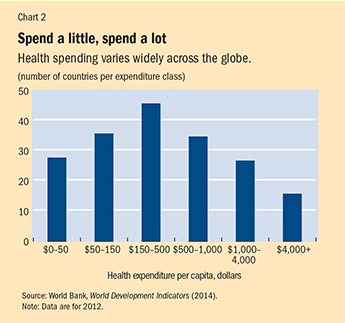
• In 2012, 28 countries (mostly in sub-Saharan Africa, representing approximately 13 percent of the world population) spent less than $50 per capita on health care, while 16 countries (10 percent of the world population) spent more than $4,000 per capita (see Chart 2). Norway spent the most, at $9,055 per capita—about 600 times the $15 per capita spent by Eritrea at the other end of the spectrum.
Health matters
The American philosopher Ralph Waldo Emerson famously wrote in 1860 that “the first wealth is health.”
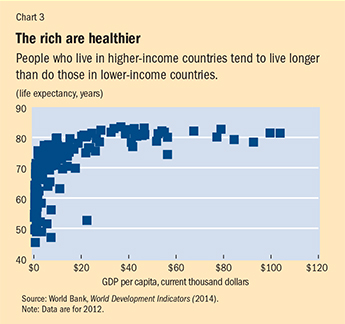
Health matters because people value living a long life that is as free as possible of physical and mental impairment. Development economists routinely illustrate the well-established connection between income and health, which is shown on a country-level basis in Chart 3. Countries with higher incomes tend to have healthier populations, traditionally seen as the result of the superior nutrition and the better access to safe water, sanitation, and health care that higher income brings.
But beyond one’s individual health, the health of others also matters, for reasons that include moral, ethical, and humanitarian concerns and human rights law. Public health also matters because of the contribution it makes to building socially cohesive and politically stable societies. For example, the inability of governments to satisfy their people’s basic health needs erodes trust and may lead to repeated cycles of instability and collapse. This is one reason why the United Nations Security Council in September 2014 declared Ebola not only a public health crisis but a threat to peace and security—an assessment it made years earlier about HIV/AIDS.
In recent years, economists have deepened their understanding of the economic importance of health, viewing it as a form of human capital that can be put to productive use, just like people’s knowledge and skills. Insofar as health is a fundamental determinant of the value of labor, which is the main asset most poor people possess, it is especially important to an individual’s or household’s ability to rise, or stay, above the poverty line.
The most rigorous evidence of the economic value of health comes from microeconomic analyses—because they are typically based on large sample sizes and rich measures of health and income and what determines them. In addition, many micro studies, which focus on individual health issues, are based on randomized controlled trials, widely considered the gold standard in this area. Some of the most compelling studies have shown the beneficial impacts of such things as
• deworming on school attendance and subsequent earnings in Kenya;
• iron supplementation on workforce participation, productivity, and earnings in Indonesia;
• iodine supplementation on cognitive function in Tanzania; and
• hookworm and malaria eradication on school attendance and labor earnings in the Americas during the last century.
Macroeconomic studies, which look at the big picture, are inherently less rigorous, but suggest that good general and reproductive health are powerful engines of economic growth, with GDP per capita getting an estimated 4 percent boost from each additional year of life expectancy. Several channels appear to be operative here. These include the positive effects of health on workforce productivity; school attendance, educational attainment, and cognitive function; savings rates, because people save more in anticipation of a longer retirement; and foreign direct investment, which often carries with it new technology, job creation, and increased trade. Fertility also tends to decline in a healthier population, which leads to a so-called demographic dividend of generally rising incomes, because the labor force grows faster than the portion of the population (young and old people) that depends on it.
Focus on the future
The prominence of global health has increased dramatically during the past two decades, with the subject occupying a central role as both an indicator and instrument of social and economic development.
According to a November 2013 article in The Atlantic magazine, of the top 20 innovations that have most shaped the nature of modern life since the invention of the wheel about 6,000 years ago, five are directly related to health: penicillin, optical lenses, vaccination, sanitation systems, and oral contraceptives.
Innovations in health abound. Personalized and precision medicine, fueled by advances in molecular and genetic testing, offers new possibilities for individualized prediction and treatment of disease. Technological innovations, such as the development of new or improved vaccines and drugs and genetically modified organisms, hold promise for the prevention and management of disease. The advent of digital health—including telemedicine, wearable sensors, electronic medical records, breakthroughs in our capacity to analyze large amounts of data, and new methods of transmitting health information and recommendations—opens up exciting new possibilities for higher-quality health care at lower cost. New diagnostic, assistive, and treatment devices create similar possibilities.
However, many problems must be tackled before the promise of these innovations can begin to be fully realized across the globe. To do so will require financial muscle, political will, and collaboration among many stakeholders and actors—including nongovernmental organizations, private companies, the media, academia, the medical community, and government departments in the health and related sectors—both within and between countries.
Some solutions will simply require more resources to enable health providers to take better advantage of existing knowledge about how to promote and protect health. Others will require building infrastructure for sanitation, potable water, transportation, communication, education, and energy—all of which are important ingredients in providing and accessing quality health care. Yet others will require new policies and institutional arrangements to motivate people to make positive lifestyle changes and encourage business innovation in the design and delivery of health-promoting products like vaccines and drugs and services such as medical examinations, public health messages, and surgeries. Continued scientific advances must feed those product pipelines and supply chains and address the formidable challenges presented by health threats from diseases such as Ebola; chikungunya (a viral infection spread by mosquitoes, which typically causes fever and joint pain); MRSA (methicillin-resistant staphylococcus aureus) and other antibiotic-resistant infections; and noninfectious threats such as obesity, depression, and environmental health problems (see “Global Health Threats of the 21st Century,” in this issue of F&D).
The capacity and reach of health systems must also be expanded, with new models for conducting epidemiological surveillance and for the efficient deployment of physicians, nurses, pharmacologists, community health workers, and counselors. Coordination of different actors and stakeholders, at the local, national, and global levels, will be required to avoid duplication of effort and ensure productive information sharing, rational and grounded priority setting, and technical and economic efficiency. Coordination is also required to protect health from such spillovers of economic progress and globalization as cross-border mobility, climate change, desertification, drought, and food and drug contamination.
All of these efforts will have to be undertaken in a financially responsible manner, which will be increasingly challenging as populations grow and age beyond traditional working years and as health systems expand their reach and broaden their service mandates. Fiscal problems in many countries will make it difficult for governments to devote additional resources to health (see “The Efficiency Imperative,” in this issue of F&D).
When it comes to health strategies, the notion that one size fits all is ill founded, because social structures, customs, political systems, economic capacities, and historical legacies vary so widely across countries. For example, in some cultural settings it is unacceptable for females to be examined or treated by male physicians. In others, families expect to participate actively in the provision of in-patient care. Standards for certifying medical practitioners, and even the philosophy and nature of medical practice (for example, mainstream, homeopathic, Hindu-based ayurvedic, and traditional Chinese), vary across settings as well.
Other matters that must be considered include the decentralization of national health systems (see “Going Local,” in this issue of F&D), the implementation of pay-for-performance models, and the promotion of current and future population health and well-being through contingent cash transfer approaches, which reward indigent households for taking specific actions such as vaccinating children (or keeping them in school).
Government has a natural role to play in interventions that efficiently promote socially desirable levels of health provision. Unregulated markets will find it hard to do that for reasons that include spillover effects associated with infectious diseases and the sometimes opportunistic behavior of private health providers who use their superior information and perceived status to exploit consumers by advising them to undertake unnecessary and costly procedures.
How to organize a health care system is a major issue. Whether health care systems are most efficiently and pragmatically organized vertically, as a bunch of disease- and disorder-specific programs (aimed at dealing, for example, with HIV/AIDS and malaria), or horizontally, as a unitary system to deal with all diseases and disorders, is a subject of perennial debate among health researchers and policymakers. Even though vertical programs can count the most impressive public health successes and are relatively more amenable to rigorous evaluation, there has, in recent years, been a notable policy shift from vertical to horizontal interventions (and to diagonal interventions, in which disease-specific initiatives are used to drive systemwide improvements). This shift has occurred partly from concerns that the success of vertical programs often comes at the expense of draining other parts of the health sector of critical human and financial resources. The shift also reflects the view that vertically organized health systems inefficiently duplicate infrastructure and health delivery mechanisms. Many professionals also believe that horizontal programs are better able to evolve as new health threats emerge and are better able to shape the social environment—for example, by encouraging healthy lifestyles and adherence to drug regimens.
The outbreak of Ebola fever
Scientists identified the Ebola virus in 1976, after outbreaks in the Democratic Republic of the Congo (near the Ebola River) and Sudan.
The current outbreaks in Guinea, Liberia, and Sierra Leone are associated with the Zaire species of Ebola virus disease, believed to be the most lethal of five known varieties. The current epidemic is the worst on record—perhaps by a wide margin, given severe underreporting of Ebola due to fear, stigma, and poor surveillance by public health systems.
The virus most likely crossed over to humans via contact with blood or other fluids from an infected animal. Once an infected person shows symptoms (which normally takes between several days and several weeks), the virus can be transmitted to other people via contact with bodily fluids that penetrate mucous membranes or broken skin—including after death if, for example, people don’t take proper precautions while preparing a body for a funeral. In severely understaffed, underprovisioned, and weak health systems, the fatality rate for Ebola ranges from 40 percent to 80 percent. Moreover, the disease spreads to health workers, and fewer health workers result in an elevation of morbidity and mortality from other diseases and conditions.
The outbreaks are projected to cause billions of dollars of losses both from the cost of the disease itself and from fear of contagion, which increases employee absenteeism and disrupts many economic activities. Contagion fear also spurs people to leave infected areas, which can promote transmission of the virus and makes it difficult to trace contacts.
Doctors mainly treat Ebola with drugs to address symptoms and by replenishing lost fluids. Experimental drugs that attack the virus are being tested, along with the use of blood serum from Ebola survivors.
Promising vaccines have been developed, but have yet to be tested on humans. Distributing them will likely prove challenging in settings with poor infrastructure and in which the need far outstrips the supply. The possibility that the virus will mutate is also a concern.
In addition to Guinea, Liberia, and Sierra Leone, suspected and confirmed cases have appeared in Nigeria and Senegal, though both countries rapidly controlled the outbreaks and have been declared free of Ebola virus transmission. As of this writing, spot cases have been detected in Mali, Spain, and the United States. In addition to promoting awareness of practices that put people at risk of Ebola virus infection, and encouraging infection prevention practices, the public health response to Ebola has included quarantine of suspected cases and identification, tracing, and monitoring the health of their contacts.
Private sector’s role
Private enterprise is also important to improving health and could perhaps assume an expanded role. Its strengths include effective messaging and distribution channels; the capacity for innovation, implementation, and rapid expansion; and adherence to commercial principles that promote financial sustainability. Private spending on health (over $2.9 trillion globally in 2012, of which 44 percent was direct household spending) is significant in all countries, but especially in low- and middle-income countries (see “Private vs. Public,” in this issue of F&D). The virtues of a strong private sector notwithstanding, governments must nevertheless engage in essential activities, including provision of a safety net for those not adequately served by private providers and monitoring and regulating health markets to prevent exploitation, corruption, and other malfeasance. Public-private partnerships that bring together governments, multinational bodies, and private operations to finance and provide health care are especially desirable when they achieve an efficient division of labor between the sectors.
The nature of prevention, early detection, treatment, and care activities—and the balance among them—will always matter. Disease prevention will figure prominently in the future, likely through expanded vaccination programs, smoke-free spaces, bans on tobacco advertising, the imposition of tobacco taxes, and increased emphasis on in utero and early childhood health. Early detection is crucial because diseases caught early are typically easier and less expensive to treat. Treatment—especially in older populations with their many afflictions—must take into account the interaction of conditions and drugs and shift the focus from cure to quality of life. It is also likely that the state will have to assume an increased burden of long-term care because declining fertility and the increased participation of women in the paid labor force reduce the number of family members able to provide physical care and companionship to older folks. Investment in health could deliver handsome returns and promote fiscal solvency, especially if it limits health care costs by focusing on disease prevention and early detection, helping people to work longer and more productively.
Global health governance—the increasingly large and complex architecture and interplay of institutions focused on global health—needs strengthening to promote transparency, accountability, efficiency, and more widespread, active, and coordinated participation to address the web of national health problems and solutions (see “Overseeing Global Health,” in this issue of F&D). The World Health Organization has long been the cornerstone of global health governance. But fresh and compelling versions of global partnerships have emerged in recent years—such as the World Health Organization Framework Convention on Tobacco Control, GAVI, the Vaccine Alliance (for increasing access to immunization in poor countries), and the Global Fund to Fight AIDS, Tuberculosis and Malaria (to finance prevention and treatment activities). However, new mechanisms are also needed to promote more timely and effective disease surveillance and response, international data sharing, and intellectual property standards that guarantee the private sector, especially pharmaceutical companies, appropriate financial incentives to conduct research and development while maintaining the flexibility to deal with urgent health needs among the poor.
The Millennium Development Goals (MDGs), established by the United Nations in 2000 to target improvements in poverty, education, and health, are an excellent symbol of good global health governance. Although not legally binding, the MDGs have great legitimacy because they were affirmed by 189 members of the United Nations. They also lend themselves to accountability because they are readily measured and publicized. Although it is impossible to rigorously estimate the contribution the MDGs have made to improvements in global health, they do seem to have focused the attention of the international development community on health and sparked increased health spending, especially in low-income countries. The MDGs also highlight the need for increased efforts to address hunger, child mortality and chronic undernutrition, and maternal mortality.
Health will surely remain prominent in the post-2015 development agenda, although the nature, focus, and concrete indicators of the new goal (or goals) are not yet clear. Especially interesting will be the place of noncommunicable diseases; the emphasis on process, inputs, and risk factors rather than health outcomes; and whatever lessons the world community takes from the spread of diseases like Ebola and applies in defining a new set of aspirations for global health. ■


