The Efficiency Imperative
Finance & Development, December 2014, Vol. 51, No. 4
David Coady, Maura Francese, and Baoping Shang
Public health spending must become more efficient to avoid overwhelming government coffers

Health outcomes have improved dramatically throughout the globe over the past five decades. As one example, life expectancy at birth has increased by about 11 years in high-income countries, 26 in upper-middle-income countries, 21 in lower-middle-income countries, and 20 in low-income countries.
While these improvements reflect a range of factors—including rising incomes and advances in medical technology—increases in public health spending have also been an important factor. In advanced economies, public spending increased on average from 3¾ percent of GDP in 1970 to about 7 percent in 2012. In emerging market economies, spending increased from 2¾ percent in 1995 to 3¼ in 2012, and over the same time span, spending increased from 3 percent of GDP to 3¾ percent in developing economies.
Although there are immense benefits from rising public health spending, these spending increases present fiscal difficulties for government budgets. Public health spending already accounts for a large share of the public purse and is projected to increase further (Clements, Coady, and Gupta, 2012). In advanced economies that already must reduce their deficits to address high public debt, this spending growth will add to fiscal pressures. In emerging market and developing economies, public health spending must compete with other development priorities, such as for education and infrastructure.
Many countries view improving the efficiency of public health spending as the primary way to ensure continued gains in health outcomes without generating additional fiscal pressures. Containing spending increases through efficiency improvements is also likely to be more politically palatable than forgoing improvements in health outcomes or lowering spending in other areas. The effectiveness of this strategy, however, depends on the extent of inefficiencies in the public health system and the capability of governments to reduce them.
Spending inefficiencies
Identifying the extent of spending inefficiency is difficult.
First, inefficiency is difficult to define because public health spending serves more than one objective. The World Health Organization classifies the primary objectives as improving the health of the population, protecting households from financial risk, and responding to people’s expectations. But most studies of spending inefficiency focus on health outcomes, such as some measure of life expectancy. While such studies may capture well the objective of improving health outcomes—because life expectancy is highly correlated with other health indicators of interest—they provide only a partial picture.
Second, measuring inefficiencies typically involves comparing a particular health system to an “efficient” one. Because many factors other than spending affect health, and they vary across countries, it is difficult to identify the minimum spending required to achieve given health outcomes.
Sources of inefficiency
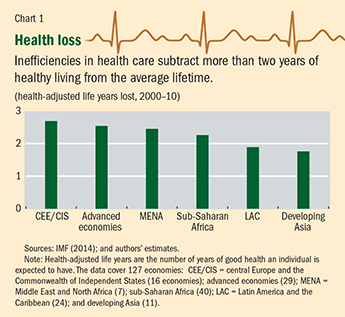
Still, studies find significant inefficiencies in the use of public resources in the health sector. The 2010 World Health Report (WHO, 2010), based on studies of health care systems worldwide, suggests that 20 to 40 percent of total (public and private) health spending in high-, middle-, and low-income countries does little to improve people’s health. A study of the countries that make up the Organisation for Economic Co-operation and Development (OECD) found that inefficiencies in those countries cut life expectancy by about two years on average (Joumard, André, and Nicq, 2010). A more recent study (IMF, 2014) that adjusts life expectancy for health quality finds that the average loss in health-adjusted life expectancy (HALE, see box) from inefficiencies is more than two years (see Chart 1). This is substantial considering that a 50 percent increase in health spending would extend HALE by about one year on average, which points to a large potential for efficiency improvements for all countries.
HALE and hearty
Health-adjusted life expectancy (HALE) represents the number of years expected to be lived in good health. A significant amount of health sector resources is spent to reduce the severity of diseases and improve the quality of people’s lives. To capture this element, HALE takes into account disease prevalence, incidence, and duration and data on a person’s years in different states of health.
These inefficiencies have numerous sources and a number of potential remedies.
Evidence for OECD countries suggests that the type of public health system does not appear to be a major factor (Joumard, André, and Nicq, 2010). Government involvement in the health sector in most countries is extensive and can take a variety of forms, including direct provision of health services, financing through the tax system, and regulation of services offered by the private sector. But when health care systems are classified according to the involvement of market mechanisms in their provision and financing, differences in efficiency within groups are found to be greater than differences across groups. This suggests that efficiency depends on more specific factors, such as what is included in the health benefit package, how private providers are reimbursed, how cost sharing is structured, and how clinical guidelines are developed and enforced.
The composition of health spending and health care services is also important. Evidence shows that primary and preventive care are in general more cost-effective than hospital care. However, even within each type of care, the cost-effectiveness of different treatments differs significantly. For example, generic drugs are as effective as brand-name drugs, but cost significantly less. A public benefit package should cover or encourage only the most cost-effective treatments.
The composition and characteristics of recipients of public health spending matter. The poor and disadvantaged are less likely to have alternative access to care if public spending is unavailable, so the gain from spending on the poor will be larger than from spending on the rich. Countries with healthier populations tend to have low health inequality.

WHO (2010) grouped the leading sources of inefficiency into five broad categories: human resources for health, which includes an inappropriate or costly staff mix and unmotivated workers; medicine, which includes underuse of generics and unnecessarily high prices for medicines, use of substandard and counterfeit medicines, and inappropriate and ineffective use of medicines; hospitals, which includes overuse of expensive medical technology (such as magnetic resonance imaging), inappropriate hospital size, and medical errors and suboptimal quality of care; waste, corruption, and fraud; and an inefficient mix and inappropriate level of treatment. Addressing all these inefficiencies could reduce total health spending by more than 40 percent on average (see Chart 2).
Addressing inefficiency
Researchers have identified several areas where reform could reduce health system inefficiency.
• Health spending should be reallocated toward the use of the most cost-effective services and treatments and provide incentives for such efficient behavior. For example, primary and preventive care—which ranges from regular doctor visits and immunization to prevention of HIV, smoking, and obesity—is often underprovided and underused. This suggests an important supporting role for government in research and development, public health care provision, regulations and clinical guidelines, and tax measures (Jamison and others, 2013). In addition, cost sharing could be designed to encourage use of more cost-effective care, particularly in emerging market and low-income countries where health insurance coverage is incomplete. These countries should seek to achieve universal coverage with a benefit package that covers only the most essential and cost-effective services, until the capacity to finance higher public health spending increases. This would not only help reduce inequality but also improve the overall health of the population.
• Governments should foster competition and choice. Such reform includes allowing competition for patients among insurers and service providers and dissemination of information on price and quality of health services. This could force health service providers to be more efficient, through such measures as an appropriate mix of doctors, nurses, and administrative staff and better use of infrastructure. Improvements in competition and choice have been shown to be positively associated with better health outcomes, although the effects on costs are less clear (Gaynor, Moreno-Serra, and Propper, 2013). Still, there is a strong role for regulation to ensure the proper functioning of the market and to limit such market failures as underprovision of health care and health insurance. This is likely more relevant for advanced economies, because a high level of administrative capacity is needed for sophisticated regulation.
• Provider payment systems must be improved. This reform includes shifting from fee-for-service payments, under which a provider is reimbursed for each service rendered, to case-based payments, such as capitation (providers receive a fixed amount for each patient under their care) and diagnosis related groups, which reimburse based on standard care for a patient’s condition. Case-based payments can help reduce incentives to provide unnecessary treatment. However, to prevent undertreatment, strong clinical guidelines and monitoring are needed. This applies to most economies that have a large private health sector.
• Modern health information technology must be adopted. Technology appears to help improve health outcomes and lower costs by reducing medical errors and duplication of procedures and tests (Hillestad and others, 2005). But large up-front investments are required, so lack of financing may constrain adoption in some countries.
• Governments must improve the operations of public institutions. Efficiency can be enhanced through consistent assignment of responsibilities across government levels (by avoiding overlap and excessive administrative costs). The development and enforcement of appropriate clinical regulations can help reduce the overuse or inappropriate use of treatments. Improving transparency and enforcement of regulations, in particular those related to procurement and reimbursement, can help reduce corruption and fraud, which appear to be significant across all economies.
Improving the efficiency of public health care spending is paramount in all economies. Reforms to enhance public spending efficiency must be tailored to each country. In advanced economies, population aging and high public debt mean that governments must stabilize or contain the increase in the ratio of public health spending to GDP without hurting health outcomes. Developing economies must continue to improve health outcomes, while preserving the sustainability of public finances. ■
David Coady is the Lead Social Spending Expert, Maura Francese is a Technical Assistance Advisor, and Baoping Shang is an Economist, all in the IMF’s Fiscal Affairs Department.
References
Clements, Ben, David Coady, and Sanjeev Gupta, 2012, Economics of Public Health Care Reform in Advanced and Emerging Economies (Washington: International Monetary Fund).
Gaynor, Martin, Rodrigo Moreno-Serra, and Carol Propper, 2013, “Death by Market Power: Reform, Competition, and Patient Outcomes in the National Health Service,” Economic Policy, Vol. 5, No. 4, pp. 134–66.
Hillestad, Richard, and others, 2005, “Can Electronic Medical Record Systems Transform Healthcare? Potential Health Benefits, Savings, and Costs,” Health Affairs, Vol. 24, No. 5, pp. 1103–117.
International Monetary Fund (IMF), 2014, Fiscal Monitor (Washington, April).
Jamison Dean T., and others, 2013, “Global Health 2035: A World Converging within a Generation,” The Lancet, Vol. 382, No. 9908, pp. 1898–1955.
Joumard, Isabelle, Christophe André, and Chantal Nicq, 2010, “Health Care Systems: Efficiency and Institutions,” OECD Economics Department Working Paper No. 769 (Paris: Organisation for Economic Co-operation and Development).
World Health Organization (WHO), 2010, World Health Report—Health Systems Financing: The Path to Universal Coverage (Geneva).


