Bill of Health
Finance & Development, December 2014, Vol. 51, No. 4
Benedict Clements, Sanjeev Gupta, and Baoping Shang
The recent slowdown in the growth of public health spending in advanced economies is not likely to last

Containing growth in public health spending is one of the most important fiscal issues facing advanced economies. Such spending has grown substantially over the past three decades (Clements, Coady, and Gupta, 2012) and accounts for about half of the increase in noninterest government spending over these years.
During the same period private health spending—which on average accounts for about a quarter of all health expenditures in advanced economies—also rose. While higher spending has coincided with enormous improvements in health, it has also put substantial pressure on budgets, particularly now, when total public debt as a percent of GDP has reached unprecedented levels in advanced economies.
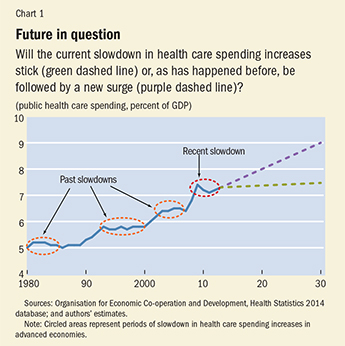
Since 2010, growth in public health care spending has slowed, and it is crucial to understand what that means. Will the slowdown persist and is health spending under control? In the past, periods of slow growth typically were followed by periods of acceleration (see Chart 1). Will this slowdown be different? The answers to these questions have important implications for the long-term economic outlook for advanced economies. Rising health care spending in those economies could force governments either to reduce spending in other priority areas (such as education and infrastructure) or slow their progress in reducing public debt—both of which could have a bearing on growth prospects in these economies.
Simultaneous slowdowns
The slowdown in the growth of public health spending that began in 2010 occurred in almost all advanced economies. Public health spending includes outlays for services provided in government hospitals and health facilities, as well as for public health insurance that pays for treatment from private hospitals, doctors, and nurses. On average, public health spending in those economies fell from 7.4 percent of GDP in 2009 to 7.1 percent of GDP in 2011. In 2012, the most recent year for which comparable data across countries are available, average public health spending rose slightly as a share of GDP. The growth of public health spending, adjusted for inflation, tells a similar story—it fell from 4.5 percent in 2009 to close to zero in 2010. While real spending growth rebounded in 2011 and 2012 it was still well below its historical average.
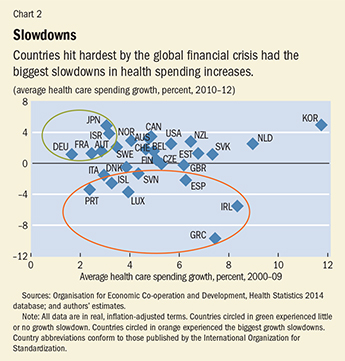
The spending slowdown was larger in countries that were hit hard by the global financial crisis and experienced sharp declines in output—Greece, Iceland, Ireland, Portugal, and Spain. But in countries less affected by the crisis—such as Germany, Israel, and Japan—spending slowed little or not at all (see Chart 2). The slowdown has touched nearly all categories of health care spending: inpatient, outpatient, pharmaceutical, preventive, and public health (Morgan and Astolfi, 2013).
The slowdown in growth for all types of spending in nearly all advanced economies—and at about the same time—suggests that it was driven by a common factor. The common element appears to be the global financial crisis, which affected economic activity and governments’ capacity to finance continued health care spending growth.
Whether the slowdown will persist depends on how the underlying drivers of spending evolve in the future. There are five main drivers.
Population aging: Health care needs typically increase as people grow older. The average age of the population in advanced economies is projected to rise over the next 20 years as a result of continued increases in life expectancy and likely will contribute to further increases in health care spending.
Income growth: Growing incomes are typically associated with rising demand for more and better health services. However, the precise value of the income elasticity (that is, the change in demand for health services in response to a change in income) is hotly debated and uncertain. Recent studies indicate that the income elasticity of demand for health care is less than or about 1.0 (Maisonneuve and Martins, 2013).
Technological advances: Improvements in medical technology are among the most important determinants of health care spending. The continued development of new procedures and medicines has dramatically expanded the prevention and treatment of medical conditions, but because the technology is expensive, it has also contributed to rapid spending growth.
The Baumol effect: Named for its progenitor, economist William J. Baumol, the effect refers to the relatively high increases in unit labor costs in sectors where it is difficult to achieve productivity gains, including in services provided by government. In manufacturing, productivity can be improved by implementing new processes that reduce the number of workers needed to produce a given level of output. In health care, however, it is difficult to improve productivity, because of the limited potential to cut the number of doctors and nurses without compromising the level of services. Salaries in health care rise in line with economy-wide averages but productivity does not, so unit labor costs rise more sharply in health.
Health policies and institutions: Health care policies and institutions can influence spending through their effects on both demand and supply. On the demand side, policy determines the coverage of public benefit packages or the degree to which patients share costs (for example, copayments for doctor visits or for prescription drugs). On the supply side, policy influences spending directly (for example, for public health clinics) or indirectly through payments to private hospitals and doctors financed by public health insurance (such as Medicare in the United States).
There is no evidence that population aging, technological advances, or the Baumol effect has changed dramatically in recent years. These factors do not likely explain the sudden slowdown in public health spending observed since 2010. Slower income growth, as a result of the recent economic crisis—or changes in health care policies and institutions—could explain the slowdown. However, it is important to distinguish between structural reforms that are designed to improve the functioning and efficiency of the health care system and measures that are temporary (but unsustainable) responses to macroeconomic and fiscal conditions. Structural changes are likely to have a lasting impact on the growth of public health spending, while the effects of temporary measures are likely to diminish as macroeconomic and fiscal conditions improve.
Immediate savings
In addition to slower income growth, the spending declines during the recent slowdown appear to reflect policies that reduced the level of spending in the short run in response to tightening macroeconomic and fiscal conditions. Thus, these policies are unlikely to influence the long-term growth of health care spending. The measures introduced in many countries were focused mainly on generating immediate savings, rather than on improving the efficiency and quality of health spending. Measures have focused on across-the-board cuts in national health budgets in Greece, Ireland, Italy, Portugal, and Spain; cuts in prices for pharmaceuticals and other medical goods in Austria, Belgium, Greece, Ireland, the Netherlands, Portugal, and Spain; reduced payments to providers in the Czech Republic, Estonia, Ireland, and Spain; and cuts in wages and salaries in the Czech Republic, Denmark, Greece, Ireland, Portugal, Slovenia, Spain, and the United Kingdom (Mladovsky and others, 2012). While these macro-level measures (so called because they affect overall spending in an untargeted manner) can help trim spending in the short run, they are less effective in containing spending growth in the long run without accompanying reforms—for example, those that introduce competition and improve incentives for providing cost-effective care (Clements, Coady, and Gupta, 2012). Furthermore, some of these macro measures, such as cuts in health promotion and disease prevention, could raise spending pressures over the longer term because their adverse effects on health could increase the need for more expensive medical interventions in the future.
Econometric analysis indicates that macroeconomic and fiscal indicators (such as economic growth, unemployment, and gross government debt) are important determinants of the growth in public health care spending because of their direct or indirect effect on some of the previously described main drivers of that spending. The analysis, based on a model using annual data for all advanced economies during 1980–2012, showed that a slowdown in economic growth and rising unemployment reduce the growth of health care spending.
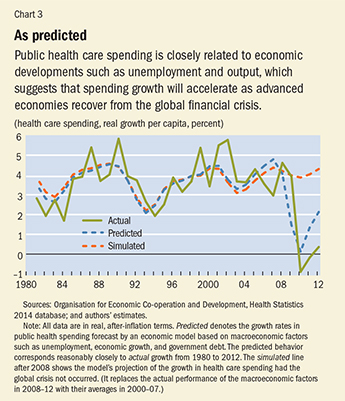
High government debt also reduces spending growth, because heavily indebted governments cannot afford to raise spending much. Nearly all of the decline in the growth of public health spending between 2008 and 2010 can be explained by these factors. For this period, the observed growth of health care spending and the value predicted by our model are very close (see Chart 3). Furthermore, the model also correctly predicts the subsequent increases in the growth of public health spending in 2011 and 2012. Had the economic crisis not occurred, the model predicts, health spending growth would have stayed largely unchanged on its precrisis path. While far from conclusive, these findings suggest that the recent slowdown is mostly temporary.
Future of spending
Available health care spending data from seven countries (Finland, Germany, Iceland, Italy, Korea, Netherlands, Norway) indicate a further increase of 0.1 percent of GDP in 2013, which is consistent with the predictions of the model. In the United States, data from the Bureau of Economic Analysis indicate faster growth in consumer spending for hospitals, nursing homes, and physician visits and other health care services during the first quarter of 2014, though some of this may be attributed to insurance expansion under the Patient Protection and Affordable Care Act (so-called Obamacare). More recent studies for the United States also suggest that the slowdown was driven mostly by economic conditions, not structural change in the health care sector (Chandra, Holmes, and Skinner, 2013; Dranove, Garthwaite, and Ody, 2014).
While the slowdown is likely to be mostly temporary, it could still have a permanent impact on public health spending in some advanced economies for two reasons:
• When the historical growth rate of public health spending resumes, that growth will be from a lower base of spending as a percent of GDP than had there been no crisis.
• Some of the macroeconomic and fiscal factors that dampen spending growth (such as high public debt ratios) are not expected to return to precrisis levels in the near future.
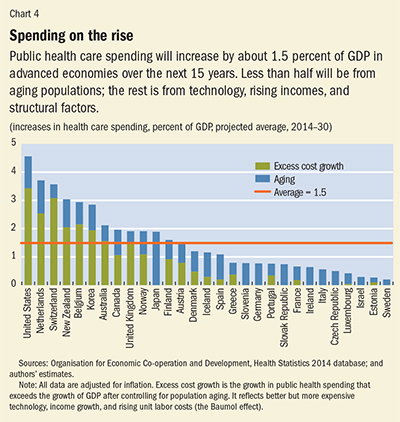
In our projections (see Chart 4), we incorporate the lower spending levels due to recent measures and assume that spending growth rates will only gradually return to historical averages as economies recover. The projections to 2019 are based on the macroeconomic projections from the IMF’s World Economic Outlook (economic growth, general government public-debt-to-GDP ratios, and unemployment rate). Beyond 2019, the projections assume that excess cost growth (the difference between the growth of real health care spending and GDP growth, after adjusting for the effect of aging) will gradually return to its historical average by 2030. On average, we project that public health spending will increase by 1½ percentage points of GDP during 2014–30. Less than half of the increase will be the result of population aging; the remainder will reflect excess cost growth because of better but more expensive technology, income growth, the Baumol effect, and health policies and institutions.
The results also suggest there will be widespread differences in spending increases across countries in the next decade and a half. In the United States, public health spending (including all health programs of the federal and state governments) is projected to increase by 4½ percentage points of GDP. Public health spending in Greece, Iceland, Ireland, Portugal, and Spain is expected to increase, on average, by less than 1 percentage point of GDP. This reflects the lingering effects of the global crisis on public finances and macroeconomic conditions in these countries.
Consequences for fiscal policy
The implications of these projections for the long-term public finances of advanced economies are considerable. To meet their own medium-term fiscal targets, these economies will have to raise revenues or further reduce spending. One way to gauge the magnitude of the required adjustment is to assess how much countries would have to raise their “primary balances” (revenues minus expenditures, excluding interest) over 2014–20 to meet their objectives. Recent estimates indicate that the required adjustment would, on average, be about 2¼ percentage points of GDP (IMF, 2014). On top of this, countries will have to contend with increased pension spending, which is expected to rise by 1 percentage point of GDP over the next 15 years because of population aging. As a result, total fiscal adjustment needs (including projected increases in health care spending) are 4¾ percentage points of GDP—a daunting figure that underscores the need to improve the efficiency of government spending, which is possible in a number of areas. These include reforms to public sector wages and employment; better aligning education spending to evolving needs, which are changing as the population ages; and targeting social benefits to low-income households, which would allow governments to meet their equity objectives at a lower cost.
When it comes to health care, advanced economies are not helpless and can take many steps to control spending and contain the rise in these outlays in years to come. Among the many potential actions are the following:
• Reforms that foster competition and choice, which could include competition among insurance and health service providers and disclosure of information on the price and quality of health services.
• Greater emphasis on primary and preventive care, which can reduce the need for more expensive care by keeping the population healthy.
• Improvements in provider payment systems to increase incentives to provide cost-effective treatment. Shifting away from simple reimbursement systems based on provider costs or services can reduce incentives for unnecessary care. Such improvements could include payments for services based on “diagnosis related groups,” which specify treatment protocols for a given set of medical conditions and an associated structure of fees.
• More widespread adoption of health information management systems to collect, store, and exchange patient data. These systems have the potential to both strengthen health outcomes and reduce costs.
In other words, health care spending is not fully under control in advanced economies, which underscores the need for long-lasting structural reforms to preserve and extend the impressive gains in health achieved in the past and reduce the growth of this spending to a more manageable pace. ■
Benedict Clements is a Division Chief, Sanjeev Gupta is a Deputy Director, and Baoping Shang is an Economist, all in the IMF’s Fiscal Affairs Department.
References
Chandra, Amitabh, Jonathan Holmes, and Jonathan Skinner, 2013, “Is This Time Different? The Slowdown in Healthcare Spending,” Brookings Papers on Economic Activity (Fall).
Clements, Benedict, David Coady, and Sanjeev Gupta, eds., 2012, The Economics of Public Health Care Reform in Advanced and Emerging Economies (Washington: International Monetary Fund).
Dranove, David, Craig Garthwaite, and Christopher Ody, 2014, “Health Spending Slowdown Is Mostly Due to Economic Factors, Not Structural Change in the Health Care Sector,” Health Affairs, Vol. 33, No. 8, pp. 1399–406.
International Monetary Fund (IMF), 2014, Fiscal Monitor (Washington, October).
Maisonneuve, Christine, and Joaquim Oliveira Martins, 2013, “A Projection Method for Public Health and Long-Term Care Expenditures,” OECD Economics Department Working Paper No. 1048 (Paris: Organisation for Economic Co-operation and Development).
Mladovsky, Philipa, Divya Srivastava, Jonathan Cylus, Marina Karanikolos, Tamás Evetovits, Sarah Thomson, and Martin McKee, 2012, “Health Policy Responses to the Financial Crisis in Europe,” Policy Summary No. 5 (Copenhagen: World Health Organization).
Morgan, David, and Roberto Astolfi, 2013, “Health Spending Growth at Zero: Which Countries, Which Sectors Are Most Affected?” OECD Health Working Paper No. 60 (Paris: Organisation for Economic Co-operation and Development).


